|
Chap
28
|
ASD
|
||
|
INCIDENCE
|
8% to 10% of CHD
in children
75% ASD2 + 20% ASD1
+ 5% SVASD + Coronary sinus ASD (more often seen with heterotaxy syndromes
and systemic venous anomalies, and isolated CS ASDs are rare (<1%)
|
||
|
F:M ratio for ASD2
is 2:1 but for
the sinus venosus ASDs it is 1:1
|
|||
|
GENETIC RISKS
|
A woman with ASD has 8% to
10% of having a child with any CHD
|
||
|
Heterozygous mutations in
TF NKX2.5/CSX were among the first
found in families with auto dom ASD2
Mutations in other TFs
such as TBX5, GATA4, GATA6, and TBX20 also associated with ASD2.
TBX5 mutations also are
responsible for Holt-Oram auto
dom with ASD2 + missing forearms + AV conduction
delay A locus on chromosome 14q12 with a missense
mutation in alpha-myosin heavy chain (MYH6),
a structural protein expressed at high levels in the developing atria, has
been linked to dominantly inherited ASD
ASD2 also
have been reported with cardiomyopathies from mutations in sarcomeric genes
|
|||
|
ASD2 also
are associated with Noonan, Down,
Klinefelter, Williams, Kabuki, Goldenhar, and Ellis-van Creveld.
|
|||
|
ENVIRONMENTAL RISKS
|
gestational diabetes,
PKU, influenza and exposure to retinoids,
NSAIDs, anticonvulsants, thalidomide, smoking, and alcohol (ASD and VSD)
|
||
|
PATHOGENESIS AND ANATOMIC FEATURES
|
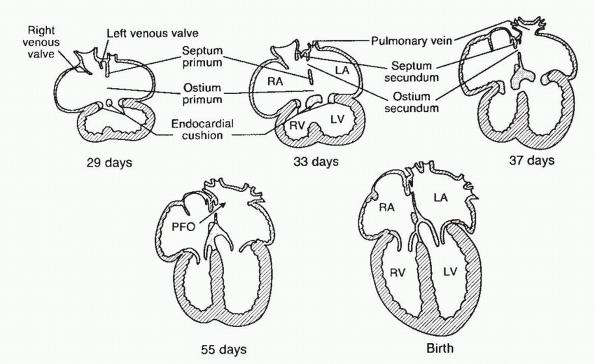
In the 4th
week of embryonic life, the septum primum appears à 5th and 6th week of embryonic life, before
complete closure of the ostium primum, tissue reabsorption occurs in the
superior portion of the septum primum resulting in another opening called the
ostium secundum
|
|
|
|
|
The septum secundum thus forms the concave-shaped superior
margin of the fossa ovalis, called the limbus
of fossa ovalis (from RA side) and the septum primum forms the valve of fossa ovalis (from LA side)
|
|
|
|
Eustachian valve
|
IVC flow from the placenta (oxygen rich) is deflected toward
the foramen ovale by the eustachian
valve
|
|
|
|
|
|
|
|
|
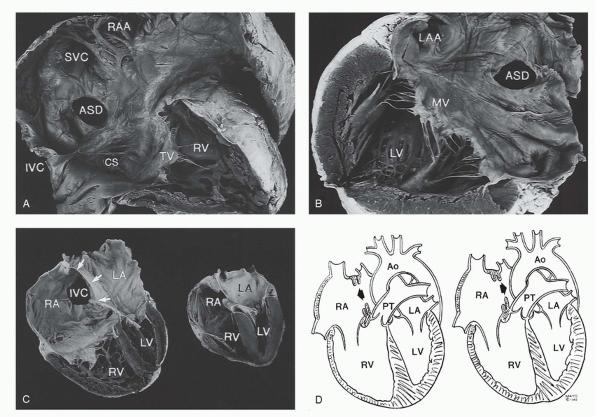
4 types of ASDs
|
D: 1= secundum ASD, 2 = primum ASD, 3 = superior SVASD, 4 = CS
ASD
|
|
|
|
ASD2
|
ASD2 occur in central part of the atrial septum (fossa ovalis)
as a result of deficient valve tissue, ectopic or excessive resorption of septum primum, or deficient growth of septum secundum
ASD2 also reported in association with noncompaction and
apical hypertrophic cardiomyopathy ApHCM
(a rare variant of HCM, described in Japanese, with usually no increase in
sudden death, although study in Toronto found that 30% have significant cards
morbidity like MI 10% or arrhythmias like A fib 12%)
|
|
|
|
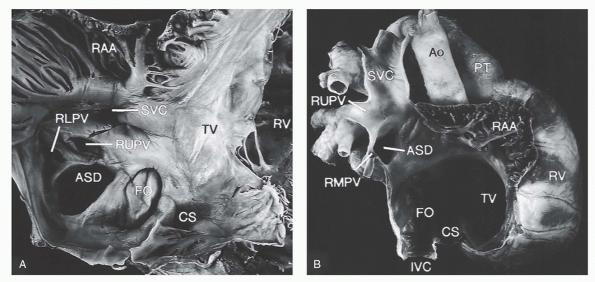
SVASD
|
SVASD defects occur outside
the margins of the fossa ovalis, in relation to the venous connections of
the RA
Ectopic or incomplete resorption of sinus venosus = deficiency
of wall btw right Pveins from the SVC, IVC, and RA
Most commonly, SVASDs are related to SVC where blood from the RUPV
or RMPV is directed into SVC or the RA.
A similar defect can occur inferior to the fossa ovalis in
relation to the IVC and RLPV orifice = IVC-type SVASD, although direct
involvement of the IVC almost never occurs. Hence, the term RA-type SVASD is
preferred
|
|
|
|
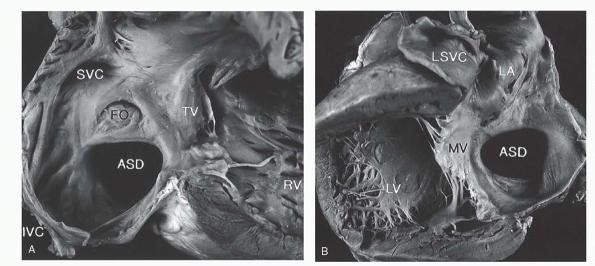
CSASD
|
The CS defect (unroofed CS) results from failure of the wall
between the LA and CS to develop. There may be complete or partial unroofing
of the CS resulting in direct communication with the LA. Almost always, this
anomaly is associated with a left SVC.
Rare complete absence of the CS rather than unroofing, blood
from the left SVC directly enters the LA.
|
|
|
|
ASSO ANOMALIES
|
ASD can be crucial for
survival in some such defects such as HLHS, D-TGA, tricuspid atresia, and
TAPVR (all cyanotic
|
|
|
|
Lutembacher $
|
association of often large and unrestrictive ASD with MS of rheumatic origin à LTR shunt is augmented from MS
|
|
|
|
PATHOPHYS
|
After birth, the lungs expand and the PBF increases. The
increased pulmonary venous return to the LA results in the left atrial
pressure exceeding the right atrial pressure causing functional closure of
the foramen ovale.
The primary determinant of the magnitude and direction of the shunt is the relative compliance of the ventricles. During
neonatal transition as the PVR drops and RV becomes thinner and more
compliant à more LTR shunt
Max LTR shunting occurs during diastole (all 4 cardiac
chambers in communication). Atrial kicks increase shunting.
During inspiration (drop intrathoracic pressure) = less blood
returns to LA à decrease LTR shunt across the ASD
Conversely, during expiration, gradient across ASD higher from
more LTR shunting
Moderate-to-large LTR shunts across an ASD à volume overload and dilation of the RA
and RV à cause TR and PR + septal bowing toward the left à abnormal LV geometry à possible MVP
increased flow into the lungs à pulm veins are dilated and there can
be flow-related pulmonary artery HTN + medial hypertrophy of PAs and
muscularization of the arterioles resulting in PVOD
With severe PVOD, patients develop Eisenmenger syndrome (RTL)
= resulting in cyanosis + syncope with
exertion
|
|
|
|
History
|
Most patients with ASD are asymptomatic and may remain
undiagnosed until later in life.
Very rarely, some infants
with ASD present with pulm overcirculation, recurrent LRIs, and FTT. Worse if
MS or MR.
Despite repair of ASD in these patients, there may not be any
significant improvement in their symptoms
|
||
|
Physical Examination
|
In patients with long-standing large LTR shunt, there is a
left precordial bulge, prominent RV impulse along LLSB
In normal hearts: during inspiration, increased venous return
into the right side of the heart à delayed P2
wide, fixed splitting of
S2 = no variation in
degree of splitting during inspiration or Valsalva
S2 is “fixed” since the increased RV stroke volume does not
vary much with respiration
A SEM due to
increased flow across the pulmonary valve (systolic ejection click means pulm
valve is truly stenotic)
When there is a large LTR shunt, a middiastolic murmur (short, soft, low to medium in frequency, and
localized to the left lower) can be heard due to excessive flow across the
tricuspid valve.
cyanosis can be seen in those with pulmonary HTN, significant RV
outflow tract obstruction, or in rare cases of a large eustachian valve
directing IVC blood into the LA via the ASD
|
||
|
EKG
|
large ASD2 showing rSR’ pattern in lead V1 and V2 and terminal
widening on S in lead V6 indicating RV volume overload
|
||
|
with SVASD
|
a frontal plane P wave axis of < 30 degrees is seen
|
||
|
With pulmonary HTN
|
the rSR’ pattern in the right
precordial leads is replaced by Q
waves and tall monophasic R waves with deeply inverted T waves (like in
ischemia)
|
||
|
older ASD2 patients
|
usually >20s, can have
junctional rhythm or atrial
arrhythmias such as atrial
fibrillation or atrial flutter.
|
||
|
EP
|
AV node dysfunction is less common than sinus node dysfunction. First-degree AV block can occur in older
individuals as a result of intraatrial H-V conduction delay and in patients
with a rare autosomal dominant form of secundum ASDs
|
||
|
Chest X-Ray
|
dilated RV - increased pulmonary vascular markings extending
to the periphery are seen in patients with significant shunts. proximal
branch pulmonary arteries, also are dilated, especially the RPA
If pulmonary HTN develops à oligemic lung fields
|
||
|
Echocardiogram
|
defining the type of ASD, its size, the degree of shunting,
its effect on the right sided chambers of the heart, associated lesions, and
estimations of RV pressure.
|
||
|
2D + M-MODE
|
Subcostal views provide the best profile of the atrial septum
since the ultrasound beam is perpendicular to it.
In apical views, a “drop-out” may be seen = a false appearance
of an ASD
PFO is guarded by a flap valve on the left side and limbus of
fossa ovalis to the right.
Sinus venosus defects are seen superiorly at the junction of
SVC with the RA
large ostium of the CS is seen as an inferior interatrial
communication, just above and anterior to the entry of IVC into RA
overloaded RV causes diastolic flattening and paradoxical
motion of the interventricular septum – shown on M-mode
|
||
|
DOPPLER
|
shunt usually is left to right, nonrestrictive = low-velocity
flow
Qp:Qs can be estimated = the time velocity integrals obtained
by tracing the pulsed-wave Doppler of pulmonary and aortic outflow are
multiplied by the area of PV and AV, respectively (unless there is RVOTO,
PDA, or AR or PR)
If PV flow gradient >
30, need to suspect additional pulm valve stenosis
PA pressure can be estimated by PR jet + RVEDP
Pulm HTN would make TR and PR worse à RVH will make RV systolic function
worse
|
||
|
TEE
|
allows better spatial resolution à adjunct for operative and percutaneous
closure of ASD.
particularly useful to detect a SVASD, which easily can be
missed using transthoracic imaging.
|
||
|
Contrast echo
|
LTR shunt is seen as a negative contrast washout into the RA
when opacified with contrast (augmented with Valsalva)
in unroofed CS, injection of contrast into left arm will have
bubble in LA before RA
|
||
|
3D echo
|
en face view of the entire atrial septum for transcatheter
device closure
|
||
|
ICE
|
device closure of ASDs, advantage of eliminating the need for
general anesthesia for TEE but require large size sheath
|
||
|
Cath
|
a step-up in oxygen saturations in RA from LTR shunt (same
when LV to RA shunt or a VSD + TR)
When the Qp:Qs
is ≥1.5, the shunt is considered significant.
PVR can be calculated = (mean PA pressure – mean LA pressure
or wedge)/Qp or cardiac output
|
||
|
CT/MRI
|
used to define the CS type of ASD, which can be particularly
challenging to recognize using routine echo in adults
Velocity-encoded,
phase-difference MRI
measurements of flow in the proximal great vessels has been used to
noninvasively measure Qp:Qs with results comparable to those obtained
by cath
|
||
|
Exercise Testing
|
Even though most patients with ASD are asymptomatic, their
exercise capacity may be decreased.
Closure of an ASD may improve exercise capacity in adults who
were asymptomatic or mildly symptomatic
helpful in documenting O2 sats during exertion if PHTN, though
maximal exercise is not recommended if severe PHTN
|
||
|
Natural History of ASDs
|
most defects <5 mm
recognized during infancy are likely to spontaneously close, but > 8 to 10 mm are unlikely to do
so. spontaneous closure occurred in all the defects that were <3 mm at diagnosis, in 87% of
defects that were 3 to 5 mm, in 80% of defects that were 5 to 8 mm, and in
none of the defects that were ≥8 mm.
|
||
|
PVOD
|
young adults c ASD have
14% chance of developing progressive PHTN à PVOD à
death from cardiac failure or PA thrombosis
When PVOD is irreversible, closure of the ASD can result in
further deterioration of the patient and decreased survival.
In most of these patients there is RV failure, and the RTL
shunt across ASD provides LV CO at the cost of cyanosis.
|
||
|
MANAGEMENT
|
anticongestive
therapy with diuretics if symptomatic
Closure of an
ASD is indicated if there is a large shunt, Qp:Qs ≥1.5, diastolic flow
rumble in the tricuspid area, RVH on EKG, cardiomegaly, increase pulm
vascular markings, RV dilation and paradoxical septal motion
If asymptomatic
large shunt, closure between 2-5 yrs,
to prevent complications such as atrial arrhythmias, paradoxical embolism,
pulmonary HTN, severe RV dilation and dysfunction with overt symptoms of CHF,
and significant MR and TR
|
||
|
Adults c ASD2
|
Late dx ASD can use a cath to determine PVR and reactivity to
pulm vasodilators.
While asymptomatic in 40s, reduced LV compliance from CAD,
HTN, valve disease à increase of the LTR shunt
Routine F/up = for atrial arrhythmias and paradoxical embolic
events and an echo q2-3 yrs to
evaluate RH size + pressure
|
||
|
Secundum ASDs
|
Surgical Closure: median sternotomy or newer partial lower sternotomy
Small ASD = direct suture
Moderate to large ASD = closure with
autologous pericardial
patch minimizing the risks of thrombosis and endocarditis
a concomitant Maze
procedure can be performed to prevent atrial arrhythmias
The overall 30-year actual survival rate among survivors of
the perioperative period was 74%, compared to 85% among age- and sex-matched
controls. However, survival is significantly decreased in those repaired
between 25 and 41 years when compared to the controls (84% and 91%,
respectively). There was a further decline in late survival in those repaired
after 41 years of age to 40% versus 59% in controls. Late repair was
associated with significant morbidity including atrial fibrillation, stroke,
and cardiac failure.
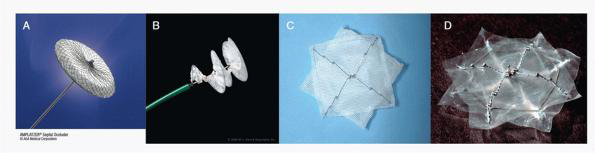
Cath
closure:
A: Amplatzer, B: Gore helex, C: cardioSEAL, D: BioSTAR
Amplatzer septal occluder is currently the most widely used
device = relatively easy deployment, easy retrievability, ability to close
large defects, and the relatively larger left atrial disc to close additional
atrial fenestrations
complications include fracture or embolization of the device,
device malalignment, residual shunts, device thrombosis, and impingement of
adjacent structures such as valves, SVC, CS, pulmonary veins, or aorta
(BioSTAR) made of collagen discs used in Europe since 2006
with very little foreign material left over at 6 months’ f/up
fully absorbable transcatheter device (BioTREK) is under trial
ASD closure at any age
was followed by improvement in symptoms and decrease in pulmonary artery pressures and right ventricular
size, but the best outcome was in patients with less functional impairment
and lower baseline PA pressures.
|
||
|
Sinus Venosus ASD
Warden procedure
|
in > 90% of cases, PAPVR to the SVC is present à surgical correction involves closure
of ASD and baffle PVeins to LA
As compared to PAPVR to RA, PAPVR connected to SVC is complex
and can be associated with long-term complications such as pulmonary vein obstruction,
SVC stenosis, sinus node dysfunction, and atrial arrhythmias (Afib or Aflutter)
When the RPveins insertion into the SVC is high (> 2 cm
above SVC/RA junction), the Warden
procedure is used, in which the SVC is transected above the site of the
anomalous pulmonary veins and connected to the right atrial appendage. The
cardiac end of the SVC along with the anomalous pulmonary venous flow is
baffled into the LA with a patch
|
||
|
Coronary Sinus ASD
|
In a partially unroofed CS defect, a roof can be created using
a pericardial patch.
If the left SVC is small and there is a bridging vein, LSVC
can be ligated.
|
||
|
Postpericardiotomy Syndrome
|
first few weeks postoperatively, patients may present with
fever, chest pain, abdominal pain, emesis, and fatigue.
echocardiogram should be performed to exclude pericardial
effusion and cardiac tamponade.
|
||
|
Pulmonary Hypertension
|
Despite closure of the defect, pulmonary vascular disease may
progress in some patients.
periodic surveillance with serial Doppler echo is recommended
to estimate PA pressures + response to pulm vasodilators
|
||
|
Atrial Arrhythmias
|
< 40 years with a prevalence of <1% à Beyond 40: 15 to 60% at 60 yo = more
likely to have higher PA pressure
periodic f/up with ECG and Holter monitoring is recommended
|
||
|
Right Atrial and Ventricular Size and Function
|
Following ASD closure, there is regression of RA and RV size
in the majority of patients, irrespective of the technique used chronic
volume overload à reduced RV systolic and diastolic function in adults, which
may or may not improve post closure
|
||
|
Left Ventricular Function
|
both systolic and diastolic function can be influenced
adversely by severe chronic RV volume overload
monitoring of both RV ad LV function during f/up is advisable.
|
||
|
Mitral Regurgitation
|
may develop MVP and MR, presumably from leftward shifting of
the ventricular septum due to an enlarged RV + MV itself often is noted to be
morphologically abnormal with myxomatous
changes and prolapse
|
||
|
Bacterial Endocarditis
|
are NOT predisposed to endocarditis
unless there is an associated valvular lesion such as cleft
mitral valve with mitral valve regurgitation
antibiotic prophylaxis is recommended for the first 6 months
following device closure and is then discontinued
|
||
|
Atrial Septal Aneurysm
|
0.22% to 1.9% = saccular deformity or protrusion >15 mm
beyond the plane of the atrial septum
commonly associated with ASD, VSD, coarc, IAA, PS, and PDA,
also arrhythmias and cryptogenic strokes – TEE helpful
|
||
|
Patent Foramen Ovale
|
present in up to 24% of healthy adults - similar in males and
females – can get larger from stretching of the fossa ovalis over time – can
be associated with cryptogenic strokes, transient ischemic attacks, and
migraine headaches – can close if needed
|
||
These notes are for personal use. They are not to be distributed or sold.
Please read Moss and Adam book for more detail information, read this at your
own risk.